Automatically write and revise medical notes that are easy to read.
Save time, reduce queries, simplify handoffs.
The only AI that writes medical documentation like a person
See how Chartbrite compares to other writing tools
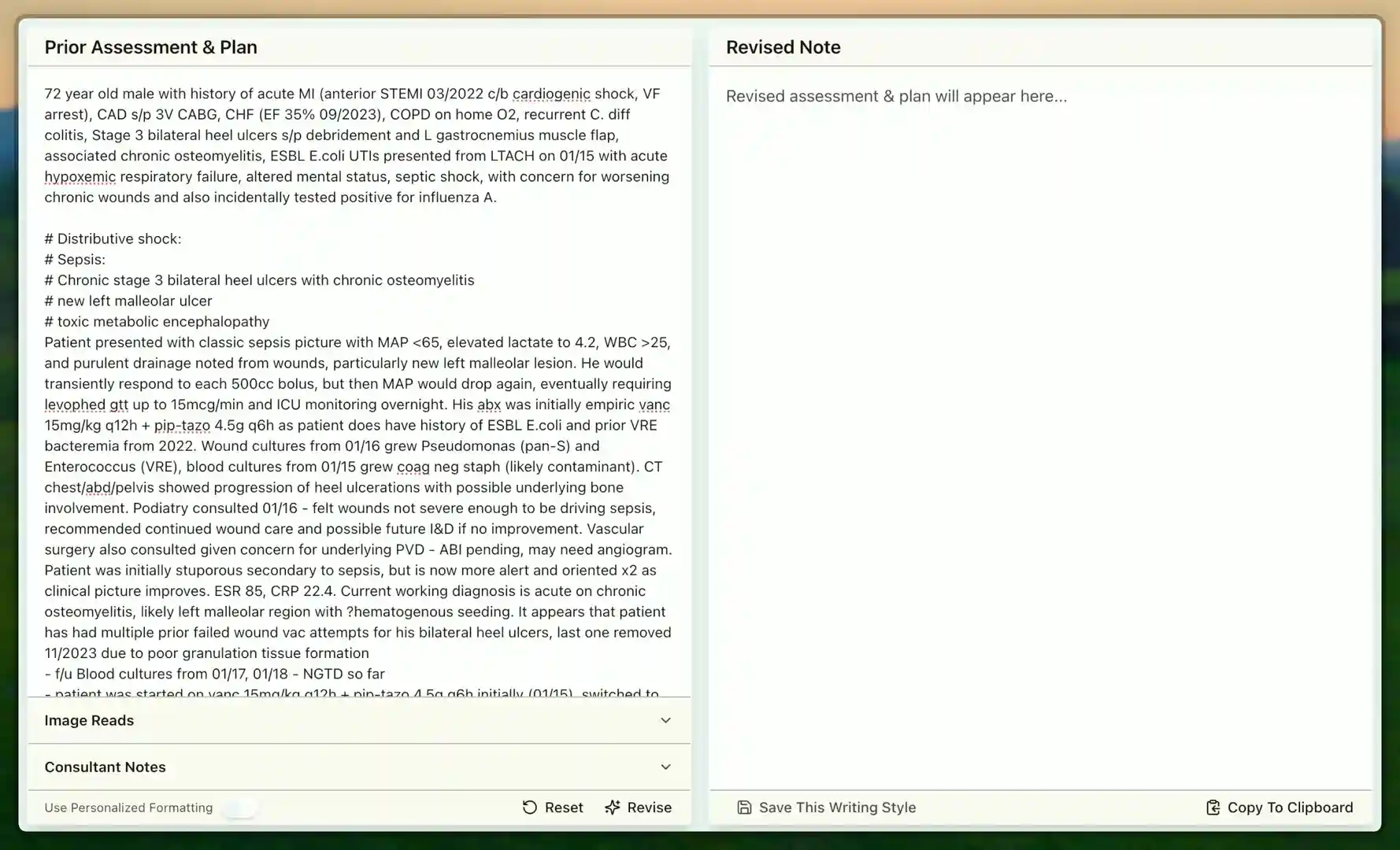
72 year old male with history of acute MI (anterior STEMI 03/2022 c/b cardiogenic shock, VF arrest), CAD s/p 3V CABG, CHF (EF 35% 09/2023), COPD on home O2, recurrent C. diff colitis, Stage 3 bilateral heel ulcers s/p debridement and L gastrocnemius muscle flap, associated chronic osteomyelitis, ESBL E.coli UTIs presented from LTACH on 01/15 with acute hypoxemic respiratory failure, altered mental status, septic shock, with concern for worsening chronic wounds and also incidentally tested positive for influenza A.
# Distributive shock:
# Sepsis:
# Chronic stage 3 bilateral heel ulcers with chronic osteomyelitis
# new left malleolar ulcer
# toxic metabolic encephalopathy
Patient presented with classic sepsis picture with MAP <65, elevated lactate to 4.2, WBC >25, and purulent drainage noted from wounds, particularly new left malleolar lesion. He would transiently respond to each 500cc bolus, but then MAP would drop again, eventually requiring levophed gtt up to 15mcg/min and ICU monitoring overnight. His abx was initially empiric vanc 15mg/kg q12h + pip-tazo 4.5g q6h as patient does have history of ESBL E.coli and prior VRE bacteremia from 2022. Wound cultures from 01/16 grew Pseudomonas (pan-S) and Enterococcus (VRE), blood cultures from 01/15 grew coag neg staph (likely contaminant). CT chest/abd/pelvis showed progression of heel ulcerations with possible underlying bone involvement. Podiatry consulted 01/16 - felt wounds not severe enough to be driving sepsis, recommended continued wound care and possible future I&D if no improvement. Vascular surgery also consulted given concern for underlying PVD - ABI pending, may need angiogram. Patient was initially stuporous secondary to sepsis, but is now more alert and oriented x2 as clinical picture improves. ESR 85, CRP 22.4. Current working diagnosis is acute on chronic osteomyelitis, likely left malleolar region with ?hematogenous seeding. It appears that patient has had multiple prior failed wound vac attempts for his bilateral heel ulcers, last one removed 11/2023 due to poor granulation tissue formation
- f/u Blood cultures from 01/17, 01/18 - NGTD so far
- patient was started on vanc 15mg/kg q12h + pip-tazo 4.5g q6h initially (01/15), switched to vanc + cefepime 2g q8h on 01/17 after culture results, ID now recommends switching to linezolid 600mg q12h + ceftazidime 2g q8h given VRE coverage needed and Pseudomonas sensitivities, plan 6-8 week course per ID recs
- Bone biopsy being considered by ortho if no clinical improvement in 48-72hrs
- ID consulted, following daily, appreciate ongoing recs
--> Foley catheter was changed out 01/15, urine culture negative
- wound care consulted 01/17, recommend daily wet-to-dry dressing changes, considering wound vac placement again if wound bed improves
- plastics consulted for possible future flap coverage
# Acute on chronic hypoxemic respiratory failure, influenza A
Patient initially required 4L NC, but he is now down to 2L NC, saturating 94% on current settings. Also note patient is on home O2 2L continuous for COPD baseline. CTA chest negative for PE or consolidation suggestive of pneumonia. ABG from 01/16: 7.38/52/78 on 2L NC. Started on tamiflu 75mg BID x5 days for influenza A. Chest PT consulted for pulmonary hygiene given copious secretions.
- continue current respiratory support, wean as tolerated
- incentive spirometry q2h while awake
- consider BiPAP trial if increased work of breathing
#?productive cough with thick yellow sputum
Not directly witnessed by nursing staff yet. Information per daughter, and according to her, this has been ongoing since his bronchoscopy procedure in November. He has been coughing up significant amounts of thick yellow material intermittently. Per her description, these can be quite voluminous episodes. She remains very concerned about this development. CT chest here unremarkable for acute process
- monitor for similar episodes during admission and consider pulmonary consult vs discussing bronchoscopy complications with pulm as clinically indicated
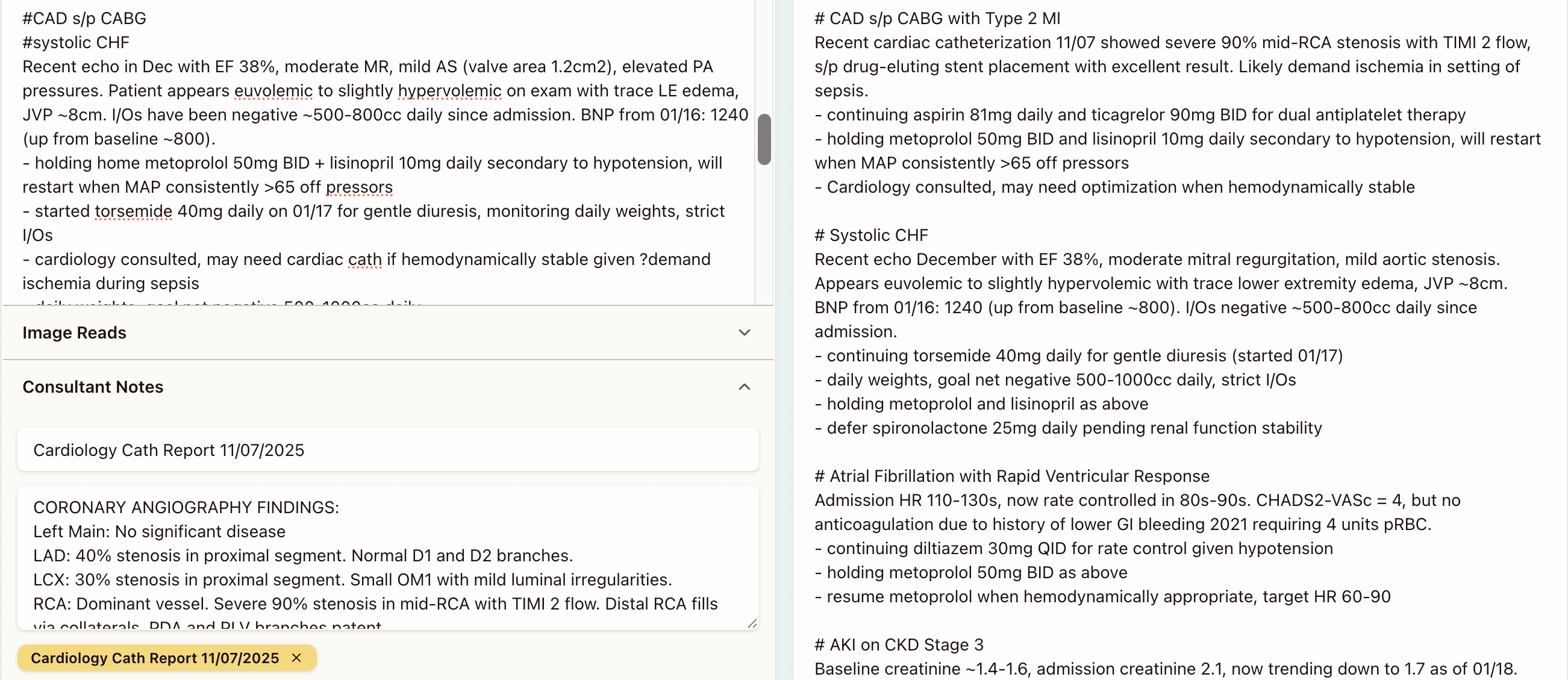
#CAD s/p CABG
#systolic CHF
Recent echo in Dec with EF 38%, moderate MR, mild AS (valve area 1.2cm2), elevated PA pressures. Patient appears euvolemic to slightly hypervolemic on exam with trace LE edema, JVP ~8cm. I/Os have been negative ~500-800cc daily since admission. BNP from 01/16: 1240 (up from baseline ~800).
- holding home metoprolol 50mg BID + lisinopril 10mg daily secondary to hypotension, will restart when MAP consistently >65 off pressors
- started torsemide 40mg daily on 01/17 for gentle diuresis, monitoring daily weights, strict I/Os
- cardiology consulted, may need cardiac cath if hemodynamically stable given ?demand ischemia during sepsis
- daily weights, goal net negative 500-1000cc daily
- consider adding spironolactone 25mg daily if renal function stable
# AFib
Patient in AFib with RVR on admission, HR 110-130s, now rate controlled in 80s-90s with current regimen. No anticoagulation due to h/o lower GI bleeding 2021 (massive LGIB requiring 4u PRBC, colonoscopy showed bleeding diverticulosis). CHADS2-VASc = 4, but bleeding risk too high per cardiology and GI.
- holding home metoprolol 50mg BID as noted above due to hypotension
- started diltiazem 30mg QID for rate control given hypotension, may uptitrate as tolerated
- resume metoprolol when hemodynamically appropriate, target HR 60-90
#h/o PE
Not on baseline anticoagulation secondary to h/o GI hemorrhage as above. Also documented allergy to warfarin (reported rash). Last PE was 2020, unprovoked, was on apixaban x 6 months until GI bleed occurred.
- enoxaparin 40mg daily for VTE prophylaxis (renal dosing given CrCl ~45)
- sequential compression devices
- early mobilization as tolerated
# AKI on CKD stage 3
Baseline creatinine ~1.4-1.6, admission creatinine 2.1, now trending down to 1.7 as of 01/18. Likely pre-renal secondary to sepsis/hypotension.
- trend creatinine daily
- renally dose medications as appropriate
- avoiding nephrotoxic agents when possible
- urine lytes from 01/16 consistent with pre-renal picture (FeNa <1%)
# DM2
Patient on home insulin glargine 24u qHS + humalog sliding scale. Sugars have been running 180-250s during sepsis. Endocrine consulted.
- continue home glargine, increase sliding scale per endo recs
- check A1c (last one 8.2% from 10/2023)
- diabetic diet when taking PO
72-year-old male with history of anterior STEMI complicated by cardiogenic shock, 3-vessel CABG, systolic heart failure (EF 35%), COPD on home oxygen, recurrent C. diff colitis, and chronic bilateral heel ulcers with osteomyelitis presented from LTACH 01/15 with septic shock, acute hypoxemic respiratory failure, and altered mental status. Remains hospitalized for ongoing sepsis management and wound care.
# Septic Shock
Presented with MAP <65, lactate 4.2, WBC >25, and purulent drainage from wounds, particularly new left malleolar lesion. Required levophed up to 15mcg/min and ICU monitoring. Wound cultures 01/16 grew pan-sensitive Pseudomonas and VRE, blood cultures 01/15 grew coagulase-negative Staphylococcus (likely contaminant). CT imaging showed progression of heel ulcerations with possible bone involvement.
- continuing linezolid 600mg q12h and ceftazidime 2g q8h per Infectious Disease recommendations for 6-8 week course
- blood cultures 01/17, 01/18 no growth to date
- Infectious Disease consulted and following daily
- bone biopsy being considered by Orthopedics if no clinical improvement in 48-72 hours
# Chronic Stage 3 Bilateral Heel Ulcers with Chronic Osteomyelitis
# New Left Malleolar Ulcer
ESR 85, CRP 22.4. Working diagnosis is acute on chronic osteomyelitis, likely left malleolar region with possible hematogenous seeding. Multiple prior failed wound vacuum attempts, last removed 11/2023 due to poor granulation tissue formation.
- Podiatry consulted 01/16, recommended continued wound care and possible future I&D if no improvement
- Vascular Surgery consulted, ABI pending, may need angiogram
- Wound Care consulted 01/17, daily wet-to-dry dressing changes, considering wound vacuum placement if wound bed improves
- Plastic Surgery consulted for possible future flap coverage
# Acute Toxic Metabolic Encephalopathy
Initially stuporous secondary to sepsis, now more alert and oriented x2 as clinical picture improves.
- supportive care, monitor mental status
# Acute on Chronic Hypoxemic Respiratory Failure with Influenza A
Initially required 4L nasal cannula, now weaned to 2L nasal cannula with oxygen saturation 94% (baseline home oxygen 2L continuous for COPD). CTA chest negative for PE or consolidation. ABG 01/16: 7.38/52/78 on 2L nasal cannula.
- continuing oseltamivir 75mg BID x5 days for influenza A
- continuing current respiratory support, wean as tolerated
- incentive spirometry q2h while awake
- Chest Physical Therapy consulted for pulmonary hygiene
- will consider BiPAP trial if increased work of breathing
# Productive Cough with Thick Yellow Sputum of Unclear Etiology
Per daughter, ongoing since bronchoscopy procedure in November with voluminous episodes of thick yellow material. CT chest unremarkable for acute process.
- monitor for episodes during admission
- will consider Pulmonology consultation if persistent
# Coronary Artery Disease s/p CABG
# Systolic Heart Failure
Recent echo December with EF 38%, moderate mitral regurgitation, mild aortic stenosis (valve area 1.2cm²), elevated PA pressures. Appears euvolemic to slightly hypervolemic with trace lower extremity edema, JVP ~8cm. BNP 01/16: 1240 (baseline ~800).
- held metoprolol 50mg BID and lisinopril 10mg daily secondary to hypotension, will restart when MAP consistently >65 off pressors
- continuing torsemide 40mg daily for gentle diuresis (started 01/17)
- daily weights, goal net negative 500-1000cc daily, strict I/Os
- Cardiology consulted, may need cardiac catheterization if hemodynamically stable
- will consider adding spironolactone 25mg daily if renal function stable
# Atrial Fibrillation
Presented with RVR, HR 110-130s, now rate controlled 80s-90s. CHADS₂-VASc = 4, but no anticoagulation due to history of lower GI bleeding 2021 requiring 4 units pRBC.
- held metoprolol 50mg BID due to hypotension
- continuing diltiazem 30mg QID for rate control, may uptitrate as tolerated
- will resume metoprolol when hemodynamically appropriate, target HR 60-90
# History of Pulmonary Embolism
Last PE 2020, unprovoked. Not on baseline anticoagulation secondary to GI hemorrhage history and documented warfarin allergy (rash).
- continuing enoxaparin 40mg daily for VTE prophylaxis (renal dosing given CrCl ~45)
- sequential compression devices
- early mobilization as tolerated
# Acute Kidney Injury on Chronic Kidney Disease Stage 3
Baseline creatinine 1.4-1.6, admission creatinine 2.1, now trending down to 1.7 as of 01/18. Likely prerenal secondary to sepsis/hypotension. Urine electrolytes 01/16 consistent with prerenal picture (FeNa <1%).
- trend creatinine daily
- renally dose medications as appropriate
- avoiding nephrotoxic agents when possible
# Severe Malnutrition
Lost 30 pounds over 3 weeks from 220 to 190 pounds. Finishes less than 10% of meals. Pitting lower extremity edema likely from anasarca due to low protein.
- nutrition consultation pending
- monitor albumin and prealbumin levels
# Diabetes Mellitus Type 2
Home insulin glargine 24 units qHS plus humalog sliding scale. Sugars running 180-250s during sepsis. Last A1c 8.2% from 10/2023.
- continuing home glargine, increased sliding scale per Endocrinology recommendations
- will check A1c
- diabetic diet when taking PO
- Endocrinology consulted
Incorporate new information directly into your new note
Chartbrite automatically integrates relevant findings